Theme: Revolutionizing Respiratory Care: Breath Well, Live Healthier
Respiratory 2020
- About The Conference
- Who Should Attend?
- Why Should Attend?
- Abstract Eligibility Criteria
- Market Analysis
- Manjor Sessions
- Past Conference Report
- Abstract Submission Deadlines
Conference Series is hosting the 11th Annual Congress on Pulmonology & Respiratory Medicine (Respiratory-2020) during March 18-19, 2020 | Amsterdam, Netherlands. The Respiratory Conference is based on the theme "Revolutionizing Respiratory Care: Breath Well, Live Healthier".
Respiratory Conference welcomes pulmonologists and Respiratory Medicine specialists across the globe to discuss current trends in respiratory disease screening to diagnosis, treatment and management. Strategic sessions of the Pulmonary & Respiratory Medicine covering about almost all of the Respiratory Diseases such as COPD, Asthma, Allergy, cystic fibrosis, pneumonia, tuberculosis, emphysema, Lung Cancers, complicated chest infections, pulmonary fibrosis, Sleep Apnea, Interstitial lung disease, Lung nodules , chronic cough, Influenza, mycobacterial infection , Paediatric Pulmonary, Bronchiectasis, and Critical Care etc.
This Pulmonology & Respiratory care Congress composed of well-organized scientific sessions, plenary sessions, Oral presentations, Poster presentations, one to one meetings, networking sessions, e-poster presentation, Young Researcher Forums (YRFs), B2B meetings, International workshops, Symposiums, Industrial sessions, Exhibitor presentations etc.
Respiratory Medicine Conference 2020 welcomes the multidisciplinary medical professionals, clinicians, and researchers associated with the diagnosis, treatment associated with the diagnosis, treatment and management of respiratory diseases and allied fields. This Respiratory Congress is the best platform that would help the Pulmonologists and Respiratory care professionals to get the insights and latest trends to improve the patients care. All the researchers working in the field of Pulmonology, Respiratory Medicine, Asthma, Pneumonia, emphysema, tuberculosis, COPD, lungs diseases, Lung Cancer, complicated chest infections and other allied fields will be of interest. The Scope of this Pulmonology & Respiratory Medicine Conference is for the below professionals, but not limited to:
- Pulmonologists
- Respiratory medicine
- Respiratory physicians
- Respiratory disease specialists
- Allergy and Immunology
- General Medicine & Internal Medicine
- Respiratory Therapy
- Radiology & Radiotherapy
- Physiotherapy
- Nursing
- Behavioural Science
- Environmental and Occupational Health
- Infectious Disease
- Paediatric Pulmonary, Critical Care, and Sleep
- Cardiology
Respiratory 2020 Conference Netherlands will enlighten the participants by providing the latest clinical updates, recent advancements in the arena of pulmonology & Respiratory care. This Respiratory Congress will help the physicians and practitioners globally to share their experience and to adopt the best practices, to strengthen the clinical collaborative research and to network among each other. Eminent Speakers, discussion on novel technologies and modern updates in the lung and respiratory system are the unique attribution of this Respiratory Conference. Dedicates sessions on Pulmonology, Respiratory care, COPD, Asthma will further help the participants to upgrade their knowledge.
By attending the Respiratory Congress 2020, Amsterdam, Netherlands can get the insights of:
- Recent trends & techniques of Respiratory Medicine & Critical care
- Upgrade yourself with latest innovations to optimize the treatment process of Respiratory Diseases
- Discuss the current challenges & update with future opportunities in improving respiratory care in future era
- Assess the treatment gaps of various pulmonary & Respiratory diseases
- Update yourself with new strategies of diagnosing Sleep Apnea, Asthma, Allergy, COPD and other related diseases and define the new treatment strategies
- Review the efficacy of spirometer access of breathing partten and to identify various disease conditions like Asthma, COPD, pulmonary fibrosis, cystic fibrosis and to optimize the non-invasive mechanical ventilation process in case of respiratory failure.
AUTHOR ELIGIBILITY:
- Individuals may submit up to two regular abstracts as the first author.
- Individuals may submit an unlimited number of Trials in Progress abstracts.
- Individuals may serve as a co-author on an unlimited number of abstracts.
ABSTRACT ELIGIBILITY
- All types of Pulmonologists, Thoracic Surgeon’s, Medicinal, Health research are eligible for submission.
- Abstract should address scientific questions, detail clinical observations, or contain primary scientific data.
- Data from the long-term follow-up of previously presented clinical trials may be submitted only if significant new information can be shown.
- Interim analysis of a prospective randomized clinical trial will be considered if it is performed as planned in the original protocol and is statistically valid.
- Abstracts of clinically-related subjects should be combined into a single abstract.
Note: Submission of multiple abstracts on a single study may result in the rejection of one or more abstracts.
Submission Requirements
Provide your full name, academic degree(s), institution, address, and email address and recent photograph. You will receive all future correspondence from us regarding the status of your abstract.
The selected abstracts will be published in Conference Proceedings.
Important Dates:
Early Bird Discount Registration Offer: On/Before Dec 15, 2019
Early Bird Abstract Submission Date: Dec 30, 2019
Abstract Submission Deadline: January 20, 2020
Speaker Presentations Sessions and Time limits:
Keynote Speech 40-45 Minutes,
Workshop/Symposium 60 Minutes
Plenary Speech 20-25 Minutes,
Poster Presentation 10-15 Minutes
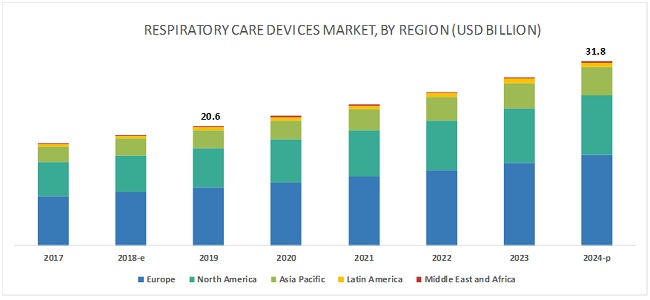
The global respiratory drugs market size will grow by USD 17.67 billion during 2018-2022. This industry research report provides a detailed analysis of the market based on type (asthma, chronic obstructive pulmonary disease (COPD), allergic rhinitis, cystic fibrosis, idiopathic pulmonary fibrosis, and other respiratory disorders.
The increase in incidences and prevalence of respiratory disorders is driving global respiratory drugs market. Several types of respiratory diseases such as COPD, asthma, and acute respiratory infections are on the rise causing major mortality and disease burden on patients. Moreover, respiratory diseases account for more than millions of deaths in developing countries with a high number of cases reported for children. This created the need for management and treatment of respiratory diseases, which in turn, drives the respiratory drugs market.
The respiratory care devices market is segmented into three major end user segments—hospitals, home care settings, and ambulatory care centers. In 2019, hospitals accounted for the largest market share of the market, mainly because of their financial capabilities, which allow them to purchase high-priced instruments and the availability of trained professionals to operate these instruments have ensured the high share of hospitals in this market. Home care settings are expected to witness the highest growth during the forecast period, mainly due to the development of compact and lightweight respiratory care devices that are easier to carry and operate.
Primary Research
In the primary research process, various sources from both supply and demand sides were interviewed to obtain qualitative and quantitative information for this report. The primary sources from the supply side include industry experts such as CEOs, vice presidents, marketing and sales directors, technology & innovation directors, and related key executives from various key companies operating in the market. The primary sources from the demand side include experts from hospitals & clinics, long term care centers, and ambulatory care centers.
Secondary Research
This research study involved the use of widespread secondary sources; directories; databases such as D&B Hoover’s, Bloomberg Business, and Factiva; white papers; annual reports; companies’ house documents; and SEC filings. Secondary research was used to identify and collect information for this extensive, technical, market-oriented, and commercial study of the global respiratory care devices market. It was also used to obtain important information about the top players, market classification, and segmentation according to industry trends to the bottom-most level, geographic markets, key developments related to market, and technology perspectives. A database of the key industry leaders was also prepared using secondary research
- Chronic Obstructive Pulmonary Disease
- Obstructive Sleep Apnea
- Pulmonary Hypertension
- Tuberculosis
- Lung Transplantation
- Asthma and Allergy
- Interstitial Lung Disease
- Pneumonia
- Lung cancer
- Paediatric Pulmonology & Critical care
- Airway and Therapeutic Devices
- Pulmonary Rehabilitation
- Cardio Pulmonary Disorders
- Pulmonary diseases: Treatment, Diagnosis and therapies
Track 01: Chronic obstructive Pulmonary Disease
Chronic obstructive Pulmonary Disease is a constant incendiary lung illness that causes discouraged wind stream from the lungs. Side effects incorporate breathing trouble, hack, bodily fluid creation and wheezing. It's brought about by long haul introduction to disturbing gases or particulate issue, frequently from tobacco smoke. Individuals with COPD are at expanded danger of creating coronary illness, lung malignancy and an assortment of different conditions. The top reason for COPD is tobacco smoking. Long haul introduction to synthetic aggravations can likewise prompt COPD. It's a sickness that generally sets aside a long effort to create
Diagnosis usually involves imaging tests, blood tests, and lung function tests. There's no solution for COPD, yet treatment can help ease manifestations, bring down the opportunity of intricacies, and for the most part improve personal satisfaction. Meds, supplemental oxygen treatment, and medical procedure are a few types of treatment. Early indications incorporate into COPD are incidental brevity of breath, particularly after exercise, mellow however repetitive hack and expecting to make a sound as if to speak regularly, particularly before anything else
Track 02: Obstructive sleep apnea
Obstructive sleep apnea is a potentially serious sleep disorder. It causes breathing to repeatedly stop and start during sleep. There are several types of sleep apnea, but the most common is obstructive sleep apnea. This type of apnea occurs when the throat muscles intermittently relax and block airway during sleep. A noticeable sign of obstructive sleep apnea is snoring.
This occurs when the muscles in the back of throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate, the tonsils, the side walls of the throat and the tongue. When the muscles relax, airway narrows or closes as you breathe in. When can't get enough air, which can lower the oxygen level in the blood.
Track 03: Pulmonary Hypertension
Pulmonary hypertension is a type of high blood pressure that affects the arteries in lungs and the right side of heart. In one form of pulmonary hypertension, tiny arteries in lungs, called pulmonary arterioles, and capillaries become narrowed, blocked or destroyed. This makes it harder for blood to flow through lungs, and raises pressure within lungs' arteries. As the pressure builds, the heart's lower right chamber (right ventricle) must work harder to pump blood through the lungs, eventually causing heart muscle to weaken and fail
Each form of Pulmonary hypertension is different, so it is important for newly-diagnosed patients to find a Pulmonary hypertension specialist who can accurately find what is causing their Pulmonary hypertension and develop a treatment plan that is right for that specific type of Pulmonary hypertension as soon as possible. Every person with pulmonary hypertension is different, and new research is being conducted every day with the potential to improve the outlook for people living with this disease. Once in the care of a pulmonary hypertension treating health care team and on appropriate therapy, people with pulmonary hypertension can live many years.
Track 04: Tuberculosis
Tuberculosis is s transferable infection that usually attacks the lungs. It can also spread to other parts of the body, like the brain and spine. A type of bacteria called Mycobacterium tuberculosis causes it. The classic symptoms of active TB are a chronic cough with blood-containing mucus, fever, night sweats, and weight loss. It was historically called "consumption" due to the weight loss. Infection of other organs can cause a wide range of symptoms. Tuberculosis is spread through the air when people who have active TB in their lungs cough, spit, speak, or sneeze. Active infection occurs more often in people with HIV/AIDS and in those who smoke. Diagnosis of active TB is based on chest X-rays, as well as microscopic examination and culture of body fluids. Diagnosis of latent TB relies on the tuberculin skin test (TST) or blood tests
Prevention of TB involves screening those at high risk, early detection and treatment of cases, and vaccination with the bacillus Calmette-Guérin (BCG) vaccine. Those at high risk include household, workplace, and social contacts of people with active TB. Treatment requires the use of multiple antibiotics over a long period of time. Antibiotic resistance is a growing problem with increasing rates of multiple drug-resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB).
Track 05: Allergic asthma
Allergic asthma is asthma caused by an allergic reaction. It’s also known as allergy-induced asthma. People with allergic asthma usually start feeling symptoms after inhaling an allergen such as pollen. The Asthma and Allergy Foundation of America reports that more than half of people with asthma have allergic asthma. Allergic asthma is treatable in most cases. An allergen is a typically harmless substance such as dust mites, pet dander, pollen or mold. If you are allergic to a substance, this allergen triggers a response starting in the immune system. Through a complex reaction, these allergens then cause the passages in the airways of the lungs to become inflamed and swollen. This results in coughing, wheezing and other asthma symptoms
The same allergens that give some people sneezing fits and watery eyes can cause an asthma attack in others. Allergic asthma is the most common type of asthma. About 90% of kids with childhood asthma have allergies, compared with about 50% of adults with asthma. The symptoms that go along with allergic asthma show up after you breathe things called allergens like pollen, dust mites, or mold. If you have asthma it usually gets worse after you exercise in cold air or after breathing smoke, dust, or fumes. Sometimes even a strong smell can set it off.
Track 06: Interstistial Lung Disease
Lung cancer is a condition that causes cells to divide in the lungs uncontrollably. This causes the growth of tumors that reduce a person's ability to breathe. In lung cancer, this pattern of cell overgrowth occurs in the lungs, which are vital organs for breathing and gas exchange. Cigarette smoking is the principal risk factor for development of lung cancer, Passive exposure to tobacco smoke (passive smoking) also can cause lung cancer in non-smokers. The two types of lung cancer, which grow and spread differently, are small-cell lung cancers (SCLC) and non-small-cell lung cancers (NSCLC). Medical professionals also refer to them as small-cell lung carcinoma and non q-small-cell lung carcinoma.
The stage of lung cancer refers to the extent to which the cancer has spread in the body. Treatment of lung cancer can involve a combination of surgery, chemotherapy, targeted therapy, immunotherapy, and radiation therapy as well as newer experimental methods. The general prognosis of lung cancer is poor because doctors tend not to find the disease until it is at an advanced stage. Five-year survival is around 54% for early stage lung cancer patients that have a tumor localized to the lungs, but only around 4% in those with advanced, inoperable lung cancer. Smoking cessation is the most important measure that can prevent the development of lung cancer
Track 07: Pneumonia
Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. A variety of organisms, including bacteria, viruses and fungi, can cause pneumonia. Pneumonia is an inflammatory condition of the lung affecting primarily the small air sacs known as alveoli. Typically symptoms include some combination of productive or dry cough, chest pain, fever, and trouble breathing.
Pneumonia is usually caused by infection with viruses or bacteria and less commonly by other microorganisms, certain medications and conditions such as autoimmune diseases. Risk factors include cystic fibrosis, chronic obstructive pulmonary disease (COPD), asthma, diabetes, heart failure, a history of smoking, a poor ability to cough such as following a stroke, and a weak immune system. Diagnosis is often based on the symptoms and physical examination. Chest X-ray, blood tests, and culture of the sputum may help confirm the diagnosis. The disease may be classified by where it was acquired with community, hospital, or health care associated pneumonia
Track 08: Lung Cancer
Lung cancer is a condition that causes cells to divide in the lungs uncontrollably. This causes the growth of tumors that reduce a person's ability to breathe. In lung cancer, this pattern of cell overgrowth occurs in the lungs, which are vital organs for breathing and gas exchange. Cigarette smoking is the principal risk factor for development of lung cancer, Passive exposure to tobacco smoke (passive smoking) also can cause lung cancer in non-smokers. The two types of lung cancer, which grow and spread differently, are small-cell lung cancers (SCLC) and non-small-cell lung cancers (NSCLC). Medical professionals also refer to them as small-cell lung carcinoma and non q-small-cell lung carcinoma.
The stage of lung cancer refers to the extent to which the cancer has spread in the body. Treatment of lung cancer can involve a combination of surgery, chemotherapy, targeted therapy, immunotherapy, and radiation therapy as well as newer experimental methods. The general prognosis of lung cancer is poor because doctors tend not to find the disease until it is at an advanced stage. Five-year survival is around 54% for early stage lung cancer patients that have a tumor localized to the lungs, but only around 4% in those with advanced, inoperable lung cancer. Smoking cessation is the most important measure that can prevent the development of lung cancer
Track 09: Paediatric Pulmonology & Critical care
Respiratory implies the field of drug identifying with lung and respiratory issue. Working with general pediatrics, aspiratory pediatricians treat an extensive variety of pneumonic issue. Respiratory implies the field of solution identifying with lung and respiratory issue. Working with general pediatrics, aspiratory pediatricians treat an extensive variety of pneumonic issue. It incorporates Asthma, Sleep Disorder, Chronic Cough, Exercise initiated Asthma, Congenital Lung Problem and Pediatric Pneumonia.
A great part of the focal point of aspiratory recovery, look into and pneumonic solution goes toward the most youthful individuals from society-the babies. It's inherent however treatable. With a sound aspiratory stenosis finding the heart valve can be supplanted or repaired and kids can develop to lead ordinary solid lives. Rest apnea influences untimely infants. A circumstance called apnea of rashness exists when the tyke doesn't breath for 20 seconds or more. It's a pneumonic illness that can be treated with ventilation machines and medicines.
Track 10: Airway and Therapeutic Devices
Positive airway pressure (PAP) therapy is a generic term applied to all sleep apnea treatments that use a stream of compressed air to support the airway during sleep. With PAP therapy, you wear a mask during sleep. A portable machine gently blows pressurized room air from into your upper airway through a tube connected to the mask. This positive airflow helps keep the airway open, preventing the collapse that occurs during apnea, thus allowing normal breathing. For optimal improvement, it's important to use your PAP machine every time you sleep including naps. Overall PAP therapy is a safe and effective treatment; however there are a few counter-indications.
A major determining factor of upper airway patency during sleep is the activity of the genioglossus muscle. Activation of this muscle via stimulation of the hypoglossal nerve is a creative new approach for treatment of obstructive sleep apnea (OSA). Hypoglossal nerve stimulation therapy is commonly referred to as Inspire, a reference to the name of the company Inspire Medical Systems that developed the treatment, which was approved by the Food and Drug Administration in 2014
Track 11: Pulmonary Rehabilitation
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of the management and health maintenance of people with chronic respiratory disease who remain symptomatic or continue to have decreased function despite standard medical treatment. It is defined by the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. In general, pulmonary rehabilitation refers to a series of services that are administered to patients of respiratory disease and their families, typically to attempt to improve the quality of life for the patient.
Pulmonary rehabilitation may be carried out in a variety of settings, depending on the patient's needs, and may or may not include pharmacologic intervention. Pulmonary rehabilitation is generally specific to the individual patient, with the objective of meeting the needs of the patient. It is a broad program and may benefit patients with lung diseases such as chronic obstructive pulmonary disease (COPD), sarcoidosis, idiopathic pulmonary fibrosis (IPF) and cystic fibrosis, among others. Although the process is focused on the rehabilitation of the patient him/herself, the family is also involved. The process typically does not begin until a medical exam of the patient has been performed by a licensed physician
Track 13: Cardio Pulmonary Disorders
Cardiopulmonary disease is the medical term used to describe a range of serious disorders that affect the heart and lungs. The two primary tobacco-related cardiopulmonary diseases are Cardiovascular Disease (CVD) and Chronic Obstructive Pulmonary Disorder (COPD). Exposure to tobacco smoke has long been recognized as a prominent risk factor for CVD. Similarly minimizing exposure to tobacco smoke is the only effective way to prevent COPD. However, the mechanisms by which tobacco toxicants increase the risk of CVD and lead to the onset of COPD are still unclear. Despite reductions in smoking over the past decade, CVD and COPD remain the first and second leading causes of death among smokers. It is important to remember also that for every person who dies because of smoking; at least 30 people live with a serious smoking-related illness.
The emergence of e-cigarettes and other new tobacco products that deliver nicotine aerosolized in various solvents raises new critical questions regarding the potential risk for cardiopulmonary disease among users. The use of these new tobacco products has soared over the last few years, particularly among adolescents, and is expected to overtake the conventional cigarette market within the next decade. These new products deliver nicotine and chemical flavorings aerosolized in a base of propylene glycol and/or glycerin via inhalation.
Track 14: Idiopathic pulmonary fibrosis
Idiopathic pulmonary fibrosis (IPF) is a type of chronic scarring lung disease characterized by a progressive and irreversible decline in lung function. Symptoms typically include gradual onset of shortness of breath and a dry cough. Other changes may include feeling tired and abnormally large and dome shaped finger and toenails Complications may include pulmonary hypertension, heart failure, pneumonia, or pulmonary embolism. The cause is unknown. Risk factors include cigarette smoking, certain viral infections, and a family history of the condition. The underlying mechanism involves scarring of the lungs. Diagnosis requires ruling out other potential causes. It may be supported by a CT scan or lung biopsy which show usual interstitial pneumonia. It is a type of interstitial lung disease.
The cause of Idiopathic pulmonary fibrosis is unknown but certain environmental factors and exposures have been shown to increase the risk of getting Idiopathic pulmonary fibrosis. Cigarette smoking is the best recognized and most accepted risk factor for Idiopathic pulmonary fibrosis, and increases the risk of Idiopathic pulmonary fibrosis by about twofold. Other environmental and occupation exposures such as exposure to metal dust, wood dust, coal dust, silica, stone dust, biologic dusts coming from hay dust or mold spores or other agricultural products, and occupations related to farming/livestock have also been shown to increase the risk for Idiopathic pulmonary fibrosis. There is some evidence that viral infections may be associated with idiopathic pulmonary fibrosis and other fibrotic lung diseas
- Signs and symptoms for Idiopathic pulmonary fibrosis
- Causes for Idiopathic pulmonary fibrosis
- Pathogenesis of Idiopathic pulmonary fibrosis
- Diagnosis for Idiopathic pulmonary fibrosis
- Treatment for Idiopathic pulmonary fibrosis
Track 15: Occupational lung diseases
Occupational lung diseases are occupational, or work-related, lung conditions that have been caused or made by the materials a person is exposed to within the workplace. It includes a broad group of diseases, including occupational asthma, industrial bronchitis, chronic obstructive pulmonary disease, and inhalation injury, interstitial lung diseases such as pneumoconiosis, hypersensitivity pneumonitis, lung fibrosis, infections, lung cancer and mesothelioma. These diseases can be caused directly or due to immunological response to an exposure to a variety of dusts, chemicals, proteins or organisms
Asbestosis: This condition is caused when a person breathes in tiny asbestos fibers. Over time, this leads to lung scarring and stiff lung tissue. It’s often linked with construction work.
Coal dust: This is caused by inhaling coal dust. It causes lung inflammation and scarring. This can cause long-lasting lung damage and shortness of breath.
Silicosis: This condition is caused by breathing in airborne crystalline silica. This is a dust found in the air of mines, foundries, and blasting operations. It can also increase the risk for other lung diseases.
Byssinosis: This is caused by breathing in dust from hemp, flax, and cotton processing. It is also known as Brown Lung Disease. It causes chest tightness and shortness of breath.
Hypersensitivity pneumonitis: This is an allergic lung disease. It is caused by a lung inflammation that happens from breathing in many different substances. These include fungus spores, bacteria, animal or plant protein, or certain chemicals. They can come from moldy hay, bird droppings, and other organic dusts. The disease causes inflamed air sacs in the lungs.
Work-related asthma: This is caused by breathing in dusts, gases, fumes, and vapors. It causes asthma symptoms such as a chronic cough and wheezing. This condition can be reversed if found early.
Track 16: Pleural diseases
The chest also know as thoracic or pleuralcavity is a space that is enclosed by the spine, ribs, and sternum and is separated from the abdomen by the diaphragm. The chest cavity contains the heart, the thoracic aorta, lungs and oesophagus among other important organs. The wall of the chest cavity is made up of the rib cage and diaphragm. The chest cavity is lined by a thin shiny membrane called the pleura, which covers the inside surface of the rib cage and spreads over the lungs as well. Normally, the pleuron produces a small amount of fluid which serves as a lubricant to the lungs as they move back and forth against the chest wall during respiration.
Hemothorax: Accumulation of blood in the pleural cavity. Caused by Most chest trauma; other causes include pleural cancer and chest/heart surgery. Symptoms include Chest pain, shortness of breath, anxiety/restlessness, increased heart rate, respiratory failure if large
Pleural effusion: Accumulation of excess fluid in the pleural cavity; this accumulation pushes against the lung and prevents full expansion with breathing. This is one of the most common problems associated with the pleura. Caused by Congestive heart failure, lung cancer, pneumonia, tuberculosis, liver disease, pulmonary embolism, lupus, adverse reaction to specific medications. A symptom includes May be asymptomatic or produce shortness of breath and cough
Empyema: The accumulation of pus in the pleural cavity. This is a type of pleural effusion that is usually associated with pneumonia. The symptoms are those of the pneumonia in addition to shortness of breath and impaired breathing.
Pleural tumors: Malignant tumors arising from the pleura or spreading to the pleura from another site, and benign tumors arising from the pleura. Symptoms include Shortness of breath, chest pain, cough, unexpected weight loss
Pleurisy: It is Inflammation of the pleura. Caused by Infection of the respiratory system by a virus or bacteria, leak of air into pleural cavity from a punctured lung, chest injury, tuberculosis or other infection, tumor in the pleural cavity, rheumatoid arthritis, lupus, sickle cell crisis, pulmonary embolism, pancreatitis, complications from heart surgery Symptoms include Chest pain on taking a deep breath, shortness of breath, fever and/or chills, joint swelling and/or soreness, unexpected weight loss
Pneumothorax: Accumulation of air within the pleural cavity between the outside of the lung and the inside of the rib cage. Causes: Injury to the lung causing a leak of air, chronic obstructive pulmonary disease or other lung disease, tuberculosis, ruptured air blisters, mechanical ventilation Symptoms include Shortness of breath, rapid breathing.
Track 17: Pulmonary diseases: Treatment, Diagnosis and therapies
Diagnosis :
1. Spirometry is a noninvasive test to assess lung function. During the test, you’ll take a deep breath and then blow into a tube connected to the spirometer.
2. Imaging tests include a chest X-ray or CT scan. These images can provide a detailed look at your lungs, blood vessels, and heart.
3. An arterial blood gas test involves taking a blood sample from an artery to measure blood oxygen, carbon dioxide, and other important levels.
Treatment:
Smoking cessation: The most essential step in any treatment plan for COPD is to stop all smoking. It's the only way to keep COPD from getting defective which can eventually reduce ability to breathe.
Bronchodilators: These medications which usually come in an inhaler relax the muscles around airways. This can help relieve coughing and shortness of breath and make breathing easier.
Inhaled steroids: Inhaled corticosteroid medications can reduce airway inflammation and help prevent exacerbations. Side effects may include bruising, oral infections and hoarseness. These medications are useful for people with frequent exacerbations of COPD.
Phosphodiesterase-4 inhibitors: A new type of medication approved for people with severe COPD and symptoms of chronic bronchitis is roflumilast a phosphodiesterase-4 inhibitor. This drug decreases airway inflammation and relaxes the airways.
Antibiotics: Respiratory infections, such as acute bronchitis, pneumonia and influenza, can aggravate COPD symptoms. Antibiotics help treat acute exacerbations, but they aren't generally recommended for prevention.
Therapies:
Oxygen therapy: There are several devices to deliver oxygen to the lungs, including lightweight, portable units that you can take with you to run errands and get around town. Some people with COPD use oxygen only during activities or while sleeping. Others use oxygen all the time. Oxygen therapy can improve quality of life and is the only COPD therapy proven to extend life
Pulmonary rehabilitation program: These programs generally combine education, exercise training, nutrition advice and counseling. Pulmonary rehabilitation may shorten hospitalizations, increase your ability to participate in everyday activities and improve your quality of life.
The 10th Annual Congress on Pulmonology & Respiratory Medicine (Respiratory-2019) during February 27-28, 2019 | Paris, France was successfully held at Holiday Inn Paris – Marne La Vallée with a theme Revolutionizing Respiratory Care: Breathe Well, Live Healthier” was a great success where eminent keynote speakers from various reputed institutions with their resplendent presence addressed the gathering.
Thanks to all our momentous speakers, conference attendees who contributed towards the successful run of the conference.
“Respiratory 2019 witnessed an amalgamation of peerless speakers who enlightened the crowd with their knowledge and confabulated on various new-fangled topics related to the fields of Healthcare.
The meeting was carried out through various sessions, in which the discussions were held on the following major scientific tracks:
- Chronic Obstructive Pulmonary Disease
- Lung Transplantation
- Pulmonary Hypertension
- Lung Cancer: Screening, Diagnosis & Treatment
- Asthma and Allergy
- Pneumonia
- Chronic Bronchitis
- Emphysema
- Thoracic Tumors
- Pulmonary diseases: Treatment, Diagnosis and therapies
- Paediatric Pulmonology & Critical care
- Airway and Therapeutic Devices
- Pulmonary Rehabilitation
- Respiratory Tract Infections
- Cardio Pulmonary Disorders
- Respiratory and sleep Medicine
Respiratory 2019 Organizing Committee would like to thank the Moderator of the conference, Bashayer abahussain who has contributed a lot for the smooth functioning of this event.
Respiratory 2019 extends its warm gratitude to all the Keynote Speakers of the event:
- Prof. Alexander D Verin, Augusta University, USA
- Prof. Mohammed Ranavaya, Marshall University, USA
Conference Series is privileged to felicitate Respiratory 2019 Organizing Committee and Chairs who supported for the success of this event. Conference Series would like to thank every individual participant for the enormous exquisite response. This inspires us to continue organizing events and conferences for further research in the field of Healthcare.
With the valuable feedback received from the participants of Respiratory 2019, Conference Series will be glad to announce its next event i.e. 11th Annual Congress on Pulmonology & Respiratory Medicine (Respiratory-2020) during March 20-21, 2020 | Amsterdam, Netherlands.
See you soon at Netherlands
1st Abstract Submission Deadline: 31-10-2019
2nd Abstract Submission Deadline : January 20-01-2020
Final Abstract submission Dates: 30-02-2020
Conference Highlights
- Chronic Obstructive Pulmonary Disease
- Obstructive Sleep Apnea
- Pulmonary Hypertension
- Tuberculosis
- Lung Transplantation
- Asthma and Allergy
- Interstitial Lung Disease
- Pneumonia
- Lung cancer
- Paediatric Pulmonology & Critical care
- Airway and Therapeutic Devices
- Pulmonary Rehabilitation
- Cardio Pulmonary Disorders
- Pulmonary diseases: Treatment, Diagnosis and therapies
- Idiopathic pulmonary fibrosis
- Occupational lung diseases
- Pleural diseases
To share your views and research, please click here to register for the Conference.
To Collaborate Scientific Professionals around the World
| Conference Date | March 18-19, 2020 | ||
| Sponsors & Exhibitors |
|
||
| Speaker Opportunity Closed | Day 1 | ||
| Poster Opportunity Closed | Click Here to View | ||
Useful Links
Special Issues
All accepted abstracts will be published in respective Our International Journals.
- Journal of Pulmonary & Respiratory Medicine
- Chronic Obstructive Pulmonary Disease: Open Access
- Insights in Chest Diseases
Abstracts will be provided with Digital Object Identifier by