Theme: Current Challenges in Lung disorders and Innovations Therapeutics in Respiratory care
Respiratory 2021
Conference Series is hosting the 12th Annual Congress on Pulmonology & Respiratory Medicine (Respiratory-2021) during May 17-18, 2021 | Munich, Germany.
Respiratory Conference welcomes pulmonologists and Respiratory Medicine specialists across the globe to discuss current trends in respiratory disease screening to diagnosis, treatment and management. Strategic sessions of the Pulmonary & Respiratory Medicine covering about almost all of the Respiratory Diseases such as COPD, Asthma, Allergy, cystic fibrosis, pneumonia, tuberculosis, emphysema, Lung Cancers, complicated chest infections, pulmonary fibrosis, Sleep Apnea, Interstitial lung disease, Lung nodules , chronic cough, Influenza, mycobacterial infection , Paediatric Pulmonary, Bronchiectasis, and Critical Care etc.
This Pulmonology & Respiratory care Congress composed of well-organized scientific sessions, plenary sessions, Oral presentations, Poster presentations, one to one meetings, networking sessions, e-poster presentation, Young Researcher Forums (YRFs), B2B meetings, International workshops, Symposiums, Industrial sessions, Exhibitor presentations etc.
Respiratory Medicine Conference 2021 welcomes the multidisciplinary medical professionals, clinicians, and researchers associated with the diagnosis, treatment associated with the diagnosis, treatment and management of respiratory diseases and allied fields. This Respiratory Congress is the best platform that would help the Pulmonologists and Respiratory care professionals to get the insights and latest trends to improve the patients care. All the researchers working in the field of Pulmonology, Respiratory Medicine, Asthma, Pneumonia, emphysema, tuberculosis, COPD, lungs diseases, Lung Cancer, complicated chest infections and other allied fields will be of interest. The Scope of this Pulmonology & Respiratory Medicine Conference is for the below professionals, but not limited to:
- Pulmonologists
- Respiratory medicine
- Respiratory physicians
- Respiratory disease specialists
- Allergy and Immunology
- General Medicine & Internal Medicine
- Respiratory Therapy
- Radiology & Radiotherapy
- Physiotherapy
- Nursing
- Behavioural Science
- Environmental and Occupational Health
- Infectious Disease
- Paediatric Pulmonary, Critical Care, and Sleep
- Cardiology
Respiratory 2021 Conference Germany will enlighten the participants by providing the latest clinical updates, recent advancements in the arena of pulmonology & Respiratory care. This Respiratory Congress will help the physicians and practitioners globally to share their experience and to adopt the best practices, to strengthen the clinical collaborative research and to network among each other. Eminent Speakers, discussion on novel technologies and modern updates in the lung and respiratory system are the unique attribution of this Respiratory Conference. Dedicates sessions on Pulmonology, Respiratory care, COPD, Asthma will further help the participants to upgrade their knowledge.
By attending the Respiratory Congress 2021, Munich, Germany can get the insights of:
- Recent trends & techniques of Respiratory Medicine & Critical care
- Upgrade yourself with latest innovations to optimize the treatment process of Respiratory Diseases
- Discuss the current challenges & update with future opportunities in improving respiratory care in future era
- Assess the treatment gaps of various pulmonary & Respiratory diseases
- Update yourself with new strategies of diagnosing Sleep Apnea, Asthma, Allergy, COPD and other related diseases and define the new treatment strategies
- Review the efficacy of spirometer access of breathing partten and to identify various disease conditions like Asthma, COPD, pulmonary fibrosis, cystic fibrosis and to optimize the non-invasive mechanical ventilation process in case of respiratory failure.
- COVID-19 and Respiratory System
- COVID-19 and Asthma
- Chronic Obstructive Pulmonary Disease
- Lung cancer
- Pneumonia
- Cardio Pulmonary Disorders
- Idiopathic pulmonary fibrosis
- Interstitial Lung Disease
- Lung Transplantation
- Obstructive Sleep Apnea
- Occupational lung diseases
- Pulmonary diseases: Treatment, Diagnosis and therapies
- Pulmonary Hypertension
- Pulmonary Rehabilitation
- Tuberculosis
1. COVID-19 and Respiratory System
When the coronavirus receives in to the frame, it comes into touch with the mucous membranes that line nose, mouth, and eyes. The virus enters a healthful cell and uses the cell to make new virus parts. It multiplies, and the brand new viruses infect nearby cells. Think respiratory tract as an upside-down tree. The trunk is a trachea, or windpipe. It splits into smaller and smaller branches in the lungs. At the end of every department are tiny air sacs known as alveoli. This is where oxygen goes into the blood and carbon dioxide comes out.
The new coronavirus can infect the upper or lower a part of the breathing tract. It travels down in airways. The lining can become irritated and inflamed. In some cases, the contamination can reach the entire manner down into alveoli. COVID-19 is a brand new condition, and scientists are learning greater each day about what it can do on lungs. They agree with that the effects on the frame are similar to the ones of two other coronavirus diseases, excessive acute respiratory syndrome (SARS) and Middle East breathing syndrome (MERS).
- Cell invasion and viral replication in the nose
- Replication in the lung and immune system alerted
- Pneumonia
- Acute respiratory distress syndrome, the cytokine storm, and multiple organ failure
2. COVID-19 and Asthma
The coronavirus disorder 2019 (COVID-19) pandemic is scary for all human beings, but for those with bronchial asthma there's terrific worry that they'll have a worse outcome or be much more likely to get SARS-CoV-2. It is vital to know that currently there's no proof of increased infection prices in those with asthma. And even though the Centers for Disease Control and Prevention states those patients with moderate-severe asthma can be at greater hazard for more excessive disorder, there aren't any published facts to help this willpower at this time. There has been one report suggesting that asthma may increase the hazard of hospitalization from COVID-19 in 18-49 yr vintage adults; however, this is primarily based on a small quantity of patients.1 And within the opposite route are statistics from New York where bronchial asthma was under-represented in those who died from COVID-19. It is critical to recall we are managing an evolving pandemic and new statistics could trade the situation within the future.
There have been several reports that steroids are contraindicated in COVID-19 disease, so many are thinking what should humans with asthma do if their controller remedy is a steroid (inhaled or oral). However, humans with asthma are positioned on controller medicinal drugs to keep their allergies underneath control. In the current pandemic, the high-quality thing someone with bronchial asthma can do is to get and maintain their bronchial asthma under control. Stopping a controller medicine will put the character at hazard for developing a bronchial asthma exacerbation especially as we input spring hypersensitivity season. In the cutting-edge pandemic, remedy of an exacerbation will in all likelihood require going to the emergency branch or pressing care, in which the man or woman has a far better danger of being exposed to a person with COVID-19. So, in a way, by continuing to maintain bronchial asthma beneath control, the man or woman with bronchial asthma is surely reducing their hazard of exposure to COVID-19.
- How can we tell the Difference between COVID-19, the Flu, a Cold or Seasonal Allergies?
- How Does COVID-19 Spread?
- Who Is at Risk From COVID-19?
- How Can we Avoid Getting COVID-19 and Other Respiratory Infections?
- If we Think we Have COVID-19, What Should we Do?
- Should we wear a Mask or Face Covering to Prevent Spreading COVID-19?
3. Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease, commonly referred to as COPD, is a group of progressive lung diseases. The most common are emphysema and chronic bronchitis. Many people with COPD have both of these conditions. Emphysema slowly destroys air sacs in lungs, which interferes with outward air flow. Bronchitis causes inflammation and narrowing of the bronchial tubes, which allows mucus to build up. The top cause of COPD is tobacco smoking. Long-term exposure to chemical irritants can also lead to COPD. It’s a disease that usually takes a long time to develop. COPD makes it harder to breathe. Symptoms may be mild at first, beginning with intermittent coughing and shortness of breath. As it progresses, symptoms can become more constant to where it can become increasingly difficult to breathe
There’s no single test for COPD. Diagnosis is based on symptoms, a physical exam, and diagnostic test results. Treatment can ease symptoms, prevent complications, and generally slow disease progression. Your healthcare team may include a lung specialist (pulmonologist) and physical and respiratory therapists. Medications can reduce symptoms and cut down on flare-ups. It may take some trial and error to find the medication and dosage that works best for you. There’s no specific diet for COPD, but a healthy diet is important for maintaining overall health. The stronger you are, the more able you’ll be to prevent complications and other health problems
- What is COPD?
- What are the symptoms of COPD?
- What causes COPD?
- Diagnosing COPD
- Treatment for COPD
- Medications for COPD
- Diet recommendations for people with COPD
4. Lung Cancer
Lung cancer is a situation that reasons cells to divide inside the lungs uncontrollably. This reasons the growth of tumors that reduce a person's capacity to breathe. In lung cancer, this pattern of cell overgrowth occurs in the lungs, which are important organs for breathing and gasoline exchange. Cigarette smoking is the principal risk aspect for development of lung most cancers, Passive publicity to tobacco smoke (passive smoking) also can cause lung most cancers in non-smokers. The two varieties of lung most cancers, which grow and spread differently, are small-mobile lung cancers (SCLC) and non-small-cellular lung cancers (NSCLC). Medical professionals additionally talk to them as small-mobile lung carcinoma and non q-small-mobile lung carcinoma
The level of lung cancers mostly refers to the extent to which the cancer has unfold within the body. Treatment of lung cancers can involve a mixture of surgery, chemotherapy, centered remedy, immunotherapy, and radiation remedy in addition to more modern experimental methods. The wellknown diagnosis of lung most cancers is bad because medical doctors tend not to discover the disease till it is at an advanced stage. Five-year survival is around 54% for early level lung cancer sufferers that have a tumor localized to the lungs, but handiest around 4% in those with advanced, inoperable lung cancer. Smoking cessation is the most crucial measure that can save you the improvement of lung cancer
- Different types of types of lung cancer
- What are the symptoms of lung cancer?
- Stages of lung cancer
- Risk factors for lung cancer
- Lung cancer and smoking
- Diagnosing and treatment for lung cancer
- Diagnosing and treatment for lung cancer
5. Pneumonia
Pneumonia is a contamination that inflames the air sacs in a single or both lungs. The air sacs may fill with fluid or pus, causing cough with phlegm or pus, fever, chills, and problem breathing. A sort of organisms, consisting of micro organism, viruses and fungi, can cause pneumonia. Pneumonia is an inflammatory situation of the lung affecting mainly the small air sacs called alveoli. Typically symptoms encompass some mixture of efficient or dry cough, chest pain, fever, and hassle breathing.
Pneumonia is typically precipitated by using contamination with viruses or bacteria and less normally via other microorganisms, certain medicinal drugs and conditions which include autoimmune diseases. Risk elements consist of cystic fibrosis, chronic obstructive pulmonary disease (COPD), asthma, diabetes, heart failure, records of smoking, a poor potential to cough such as following a stroke, and a susceptible immune system. Diagnosis is often based on the signs and symptoms and bodily examination. Chest X-ray, blood tests, and lifestyle of the sputum may also help affirm the diagnosis. The disease may be classified via in which it was acquired with community, hospital, or health care related pneumonia
- Signs and symptoms of Pneumonia
- Cause for Pneumonia
- Risk factors for Pneumonia
- Complications for Pneumonia
- Diagnosis for Pneumonia
- Prevention for Pneumonia
6. Cardio Pulmonary Disorders
Cardiopulmonary disease is the medical term used to describe quite number critical problems that affect the heart and lungs. The two primary tobacco-associated cardiopulmonary illnesses are Cardiovascular Disease (CVD) and Chronic Obstructive Pulmonary Disorder (COPD). Exposure to tobacco smoke has long been diagnosed as a prominent chance component for Cardiovascular Disease . Similarly minimizing exposure to tobacco smoke is the most effective manner to save you COPD. However, the mechanisms by way of which tobacco toxicants increase the danger of Cardiovascular Disease and result in the onset of COPD are nonetheless unclear. Despite discounts in smoking during the last decade, Cardiovascular Disease and COPD stay the first and second main causes of death among smokers. It is important to keep in mind also that for all of us who dies because of smoking; as a minimum 30 people live with a critical smoking-associated illness.
The emergence of e-cigarettes and other new tobacco merchandise that deliver nicotine aerosolized in various solvents raises new essential questions regarding the potential risk for cardiopulmonary sickness among users. The use of this new tobacco merchandise has soared over the last few years, especially amongst adolescents, and is anticipated to overhaul the traditional cigarette market inside the next decade. These new products supply nicotine and chemical flavourings aerosolized in a base of propylene glycol and/or glycerine through inhalation.
- Experience with CPX in Selected Patient Populations
- Congenital Heart Defects, Valve Disease, and Hypertrophic Cardiomyopathy
- Left Ventricular Dysfunction Secondary to Myocardial Ischemia
- Application of CPX in the Clinical Care of Patients with Cardiopulmonary Diseases
- Prognostic Assessment of Candidates for Transplantation or Other Major Interventions
7. Idiopathic Pulmonary Fibrosis
Idiopathic pulmonary fibrosis (IPF) is a kind of persistent scarring lung disorder characterized by means of a progressive and irreversible decline in lung function. Symptoms typically encompass gradual onset of shortness of breath and a dry cough. Other changes may consist of feeling tired and abnormally massive and dome shaped finger and toenails Complications may encompass pulmonary hypertension, coronary heart failure, pneumonia, or pulmonary embolism. The reason is unknown. Risk factors include cigarette smoking, sure viral infections, and a family history of the condition. The underlying mechanism entails scarring of the lungs. Diagnosis calls for ruling out different potential causes. It may be supported with the aid of a CT test or lung biopsy which show typical interstitial pneumonia. It is a type of interstitial lung disease.
The purpose of Idiopathic pulmonary fibrosis is unknown however sure environmental elements and exposures have been proven to growth the risk of getting Idiopathic pulmonary fibrosis. Cigarette smoking is the first-rate diagnosed and maximum accepted risk issue for Idiopathic pulmonary fibrosis, and increases the danger of Idiopathic pulmonary fibrosis with the aid of about twofold. Other environmental and career exposures which includes publicity to metal dirt, wooden dust, coal dirt, silica, stone dust, biologic dusts coming from hay dust or mould spores or other agricultural products, and occupations related to farming/cattle have also been proven to boom the risk forIdiopathic pulmonary fibrosis. There is some proof that viral infections can be related to Idiopathic pulmonary fibrosis and other fibrotic lung disease
- Signs and symptoms for Idiopathic pulmonary fibrosis
- Causes for Idiopathic pulmonary fibrosis
- Pathogenesis of Idiopathic pulmonary fibrosis
- Diagnosis for Idiopathic pulmonary fibrosis
- Treatment for Idiopathic pulmonary fibrosis
8. Interstitial Lung Disease
Interstitial lung disorder (ILD), or diffuse parenchymal lung sickness (DPLD) is a collection of lung sicknesses affecting the interstitium the tissue and space around the alveoli. It worries alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur whilst an damage to the lungs triggers an abnormal healing response. Ordinarily, the frame generates just the proper quantity of tissue to repair damage, however in interstitial lung ailment, the repair manner is going awry and the tissue across the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The term interstitial lung disorder is used to distinguish these sicknesses from obstructive airways illnesses.
Interstitial lung disorder may be because of exposure to unsafe chemicals, positive medicines and scientific treatments. In most cases, the reasons are unknown. Lung damage from many ILDs is irreversible and progressive, that means it receives worse over time. In a few cases, it can be slowed by sure medications. Occasionally, people with interstitial lung disease will be recommended for lung transplants. Prolonged Interstitial lung sickness may bring about pulmonary fibrosis; however this isn't usually the case. Idiopathic pulmonary fibrosis is interstitial lung disorder for which no obvious cause may be recognized and is related to normal findings each radiographic and pathologic.
- What are the causes of Interstitial lung disorder
- Diagnosis for Interstitial lung disorder
- What are the treatments for Interstitial lung disorder
- Risk factors for Interstitial lung disorder
- Complications for Interstitial lung disorder
9. Lung Transplantation
Lung transplantation is a surgery wherein a patient's diseased lungs are partly or totally replaced by way of lungs which come from a donor. Donor lungs may be retrieved from a residing donor or a deceased donor. A residing donor can simplest donate one lung lobe. With some lung diseases, a recipient may handiest need to get hold of an unmarried lung. With other lung diseases including cystic fibrosis, it's far vital that a recipient receive lungs. While lung transplants carry positive associated risks, they can also enlarge existence expectancy and decorate the great of lifestyles for end-stage pulmonary patients.
Lung harm can regularly be dealt with medicinal drug or with unique breathing devices. But when these measures no longer lung function turns into existence-threatening, physician might suggest a single-lung transplant or a double-lung transplant. Some human beings with coronary artery ailment may want a procedure to restore blood flow to a blocked or narrowed artery in the heart, similarly to a lung transplant. In a few cases, human beings with severe heart and lung situations may want a combined heart-lung transplant
- Types of lung transplant
- Factors that may affect the eligibility for a lung transplant
- Risks factors for Lung transplantation
- Side effects of anti-rejection drugs
- Transplant requirements
10. Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a situation wherein breathing stops involuntarily for quick durations of time at some point of sleep. Normally, air flows smoothly from the mouth and nose into the lungs in any respect times. In Obstructive sleep apnea , the normal flow of air is time and again stopped all through the night. The waft of air stops because airway space within the region of the throat is too narrow. Snoring is characteristic of Obstructive sleep apnea . Obstructive sleep apnea reasons episodes of reduced oxygen deliver to the brain and other parts of the body. Sleep first-rate is poor, which causes sunlight hours drowsiness and absence of clarity within the morning. There are several forms of sleep apnea, but OSA is the maximum common. Obstructive sleep apnea is much more likely to occur in older people and those who're overweight. Evidence shows that weight reduction reasons marked improvement in symptoms. Sleeping in your again can irritate Obstructive sleep apnea
A prognosis of Obstructive sleep apnea starts offevolved with a complete records and bodily examination. A history of daylight hour’s drowsiness and snoring are essential clues. Your physician may additionally ask you to fill out a questionnaire about sunlight hours drowsiness, sleep habits, and excellent of sleep. This happens while the muscle tissues inside the again of throat relax. These muscular tissues guide the tender palate, the triangular piece of tissue putting from the smooth palate, the tonsils, the side partitions of the throat and the tongue. When the muscle groups relax, airway narrows or closes as you breathe in. When can't get enough air, that could decrease the oxygen level within the blood.
- What are the types of Obstructive sleep apnea?
- What Causes Obstructive sleep apnea?
- What Are the Signs & Symptoms of Obstructive sleep apnea?
- How Is Obstructive sleep apnea Diagnosed?
- How Is Obstructive sleep apnea Treated?
11. Occupational Lung Diseases
Occupational lung diseases are occupational, or work-associated, lung situations that have been triggered or made with the aid of the materials someone is uncovered to inside the workplace. It consists of a broad institution of illnesses, which includes occupational asthma, commercial bronchitis, chronic obstructive pulmonary disease, and inhalation injury, interstitial lung sicknesses including pneumoconiosis, hypersensitivity pneumonitis, lung fibrosis, infections, lung most cancers and mesothelioma. These illnesses may be induced directly or because of immunological response to an publicity to plenty of dusts, chemicals, proteins or organisms
Asbestosis: This condition is caused when a person breathes in tiny asbestos fibers. Over time, this ends in lung scarring and stiff lung tissue. It’s frequently linked with creation work.
Coal dirt: This is due to inhaling coal dirt. It reasons lung irritation and scarring. This can motive long-lasting lung harm and shortness of breath.
Silicosis: This condition is due to inhaling airborne crystalline silica. This is a dust observed within the air of mines, foundries, and blasting operations. It can also increase the chance for different lung sicknesses.
Byssinosis: This is due to inhaling dust from hemp, flax, and cotton processing. It is also called Brown Lung Disease. It causes chest tightness and shortness of breath.
Hypersensitivity pneumonitis: This is an allergic lung disease. It is caused by a lung inflammation that takes place from breathing in many one-of-a-kind substances. These encompass fungus spores, bacteria, animal or plant protein, or certain chemicals. They can come from moldy hay, bird droppings, and different organic dusts. The disease reasons infected air sacs within the lungs.
Work-related asthma: This is due to breathing in dusts, gases, fumes, and vapours. It reasons asthma symptoms including a chronic cough and wheezing. This circumstance can be reversed if determined early.
12. Pulmonary diseases: Treatment, Diagnosis and therapies
Diagnosis
1. Spirometry is a noninvasive test to assess lung function. During the test, you’ll take a deep breath and then blow into a tube connected to the spirometer.
2. Imaging tests include a chest X-ray or CT scan. These images can provide a detailed look at your lungs, blood vessels, and heart.
3. An arterial blood gas test involves taking a blood sample from an artery to measure blood oxygen, carbon dioxide, and other important levels.
Treatment:
Smoking cessation: The most essential step in any treatment plan for COPD is to stop all smoking. It's the only way to keep COPD from getting defective which can eventually reduce ability to breathe.
Bronchodilators: These medications which usually come in an inhaler relax the muscles around airways. This can help relieve coughing and shortness of breath and make breathing easier.
Inhaled steroids: Inhaled corticosteroid medications can reduce airway inflammation and help prevent exacerbations. Side effects may include bruising, oral infections and hoarseness. These medications are useful for people with frequent exacerbations of COPD.
Phosphodiesterase-4 inhibitors: A new type of medication approved for people with severe COPD and symptoms of chronic bronchitis is roflumilast a phosphodiesterase-4 inhibitor. This drug decreases airway inflammation and relaxes the airways.
Antibiotics: Respiratory infections, such as acute bronchitis, pneumonia and influenza, can aggravate COPD symptoms. Antibiotics help treat acute exacerbations, but they aren't generally recommended for prevention.
Therapies:
Oxygen therapy: There are several devices to deliver oxygen to the lungs, including lightweight, portable units that you can take with you to run errands and get around town. Some people with COPD use oxygen only during activities or while sleeping. Others use oxygen all the time. Oxygen therapy can improve quality of life and is the only COPD therapy proven to extend life
Pulmonary rehabilitation program: These programs generally combine education, exercise training, nutrition advice and counseling. Pulmonary rehabilitation may shorten hospitalizations, increase your ability to participate in everyday activities and improve your quality of life
13. Pulmonary Hypertension
Pulmonary Hypertension is a form of excessive blood pressure that affects the arteries in lungs and the right facet of coronary heart. In one form of pulmonary high blood pressure, tiny arteries in lungs, known as pulmonary arterioles, and capillaries come to be narrowed, blocked or destroyed. This makes it more difficult for blood to flow through lungs, and raises pressure within lungs' arteries. As the strain builds, the coronary heart's lower proper chamber (proper ventricle) must work more difficult to pump blood through the lungs, eventually causing coronary heart muscle to weaken and fail. Pulmonary hypertension is a pathophysiologic condition with many possible causes. Indeed, this condition frequently accompanies severe heart or lung condition
Each shape of Pulmonary hypertension is different, so it is important for newly-diagnosed sufferers to discover a Pulmonary hypertension expert who can accurately locate what is causing their Pulmonary hypertension and increase a remedy plan that is right for that specific kind of Pulmonary hypertension as quickly as possible. Every individual with Pulmonary hypertension is different, and new studies are being conducted every day with the capability to improve the outlook for people dwelling with this disease. Once in the care of a Pulmonary hypertension treating health care group and on appropriate therapy, humans with Pulmonary hypertension can stay many years
- Pulmonary Arterial Hypertension
- Pulmonary Hypertension Due to Left Heart Disease
- Pulmonary Hypertension Due to Lung Disease
- Pulmonary Hypertension Due to Chronic Blood Clots in the Lungs
- Pulmonary Hypertension Due to Unknown Causes
14. Pulmonary Rehabilitation
Pulmonary rehabilitation, also called breathing rehabilitation, is an important part of the control and health protection of people with persistent respiration ailment who remain symptomatic or hold to have decreased characteristic despite popular medical treatment. It is described via the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and complete intervention for patients with continual respiration diseases who're symptomatic and regularly have decreased each day lifestyles activities. In general, pulmonary rehabilitation refers to a sequence of services which are administered to patients of respiratory disorder and their families, typically to try and improve the nice of life for the patient.
Pulmonary rehabilitation may be finished in a number of settings, depending on the patient's desires, and might or won't encompass pharmacologic intervention. Pulmonary rehabilitation is typically precise to the character patient, with the objective of meeting the wishes of the affected person. It is a broad program and may benefit sufferers with lung diseases such as chronic obstructive pulmonary sickness (COPD), sarcoidosis, idiopathic pulmonary fibrosis (IPF) and cystic fibrosis, among others. Although the technique is targeted on the rehabilitation of the affected person him/herself, the family is also involved. The system generally does now not begin until a scientific examination of the affected person has been accomplished through an authorized physician.
- Where Is Pulmonary Rehabilitation Administered?
- Can Use Oxygen during Pulmonary Rehabilitation?
- Can Do Pulmonary Rehabilitation at Home?
- How Much Does Pulmonary Rehabilitation Cost?
15. Tuberculosis
Tuberculosis is s transferable infection that generally attacks the lungs. It also can unfold to other components of the body, like the mind and spine. A kind of bacteria known as Mycobacterium tuberculosis causes it. The classic signs of lively Tuberculosis are a persistent cough with blood-containing mucus, fever, night time sweats, and weight loss. It was historically known as "consumption" due to the burden loss. Infection of different organs can purpose a wide range of signs. Tuberculosis is spread through the air when humans who have active Tuberculosis in their lungs cough, spit, speak, or sneeze. Active contamination happens more often in people with HIV/AIDS and in those who smoke.
Diagnosis of energetic Tuberculosis is primarily based on chest X-rays, in addition to microscopic exam and tradition of frame fluids. Diagnosis of latent Tuberculosis is predicated on the tuberculin skin test (TST) or blood tests. Prevention of Tuberculosis includes screening the ones at high danger, early detection and treatment of cases, and vaccination with the bacillus Calmette-Guérin (BCG) vaccine. Those at high chance include household, workplace, and social contacts of humans with lively Tuberculosis. Treatment requires using multiple antibiotics over a long period of time. Antibiotic resistance is a growing problem with increasing costs of multiple drug-resistant tuberculosis (MDR-TB) and drastically drug-resistant tuberculosis (XDR-TB).
- Symptoms of Tuberculosis
- Causes for Tuberculosis
- Risk factors of Tuberculosis
- Complications of Tuberculosis
- Prevention of Tuberculosis
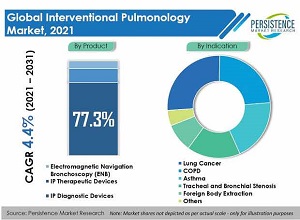
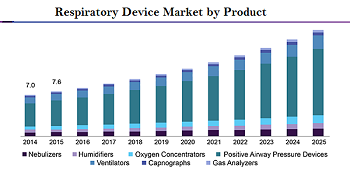
"Global Respiratory Equipment Market: Size & Forecast with Impact Analysis of COVID-19 (2020-2024)”, provides an in-depth evaluation of the global respiratory equipment market consisting of specified description of effect of COVID-19, marketplace sizing and growth. The evaluation consists of market with the aid of cost and market share by using phase, by disease, and by way of region. Furthermore, the record also provides specific section and regional evaluation.
Moreover, the document additionally assesses the key opportunities in the market and descriptions the factors which are and would be riding the boom of the enterprise. Growth of the overall international system marketplace has also been forecasted for the years 2020-2024, taking into account the previous increase patterns, the increase drivers and the present day and future trends.
Philips, ResMed Inc., Medtronic Plc, and Fisher & Paykel Healthcare are a number of the key gamers operating within the international breathing system marketplace, whose employer profiling has been done in the document. In this section of the record, enterprise evaluate, financial assessment and enterprise strategies of the respective businesses are provided.
Region Coverage
North America
Europe
Asia Pacific
ROW
Company Coverage
Philips
ResMed Inc.
Medtronic Plc
Fisher & Paykel Healthcare
Executive Summary
Respiratory device consists of clinical equipment that assists sufferers with breathing in a extreme medical situation. In addition, the devices deliver remedy to treat numerous breathing sicknesses. Moreover, respiration devices are used for prognosis of breathing problems.
Furthermore, respiratory gadgets facilitate in treatment and tracking of respiration issues. The devices are mostly used for the remedy of different respiration disorders like: obstructive conditions, neuromuscular issues, restrictive conditions, vascular illnesses and other illnesses like pneumonia, tuberculosis, asbestosis etc. Major breathing care devices include CPAP machines, transportable emergency oxygen systems, oximetry meters, nebulizers etc.
Patients with respiratory sickness are handled with one of a kind clinical gadget like: air cleaner, CPAP machines, BiPAP machines, transportable emergency oxygen systems, etc. These, device facilitate the medical experts to efficaciously and efficaciously deal with patients with intense breathing illnesses.
The international breathing gadget market has expanded progressively over time and the marketplace is further expected to propel at a regular pace at some point of the forecasted years 2020 to 2024. The market would propel as a result of one of a kind boom drivers like surging ageing population, rising healthcare expenditure, growing continual sicknesses, escalating cigarette consumption, rise in carbon emission, escalating obese populace and surging diabetic population.
However, the marketplace faces a few demanding situations which might be obstructing the growth of the market. Some of the essential challenges faced with the aid of the industry are: fast technological advancement, stringent product approval and tracking regulatory, existence of neighborhood manufacturers, loss of raw fabric availability and outcomes of breathing devices on infants.
Conference Highlights
- COVID-19 and Respiratory System
- COVID-19 and Asthma
- Chronic Obstructive Pulmonary Disease
- Lung cancer
- Pneumonia
- Cardio Pulmonary Disorders
- Idiopathic Pulmonary Fibrosis
- Interstitial lung disease
- Lung transplantation
- Occupational lung diseases
- Obstructive sleep apnea
- Pulmonary diseases: Treatment, Diagnosis and therapies
- Pulmonary Hypertension
- Pulmonary Rehabilitation
- Tuberculosis
To share your views and research, please click here to register for the Conference.
To Collaborate Scientific Professionals around the World
| Conference Date | May 25-26, 2021 | ||
| Sponsors & Exhibitors |
|
||
| Speaker Opportunity Closed | |||
| Poster Opportunity Closed | Click Here to View | ||
Useful Links
Special Issues
All accepted abstracts will be published in respective Our International Journals.
- Journal of Pulmonary & Respiratory Medicine
- Journal of Chronic Obstructive Pulmonary Disease
- Journal of Allergy & Therapy
Abstracts will be provided with Digital Object Identifier by